United States: A new trial has found that genetically modified kidneys keep monkeys alive for more than two years. In the largest of its kind trial, researchers transplanted kidneys from genetically edited pigs into monkeys that lived for a record amount of time.
According to reports, about 13 people die every day due to a lack of kidney donors. The scientists hope that the study, published in the journal Nature this week, could soon lead to human trials.
Previous studies show that about 8 percent to 16 percent of people globally have kidney problems, and more than 250,000 people died due to them in 2019.
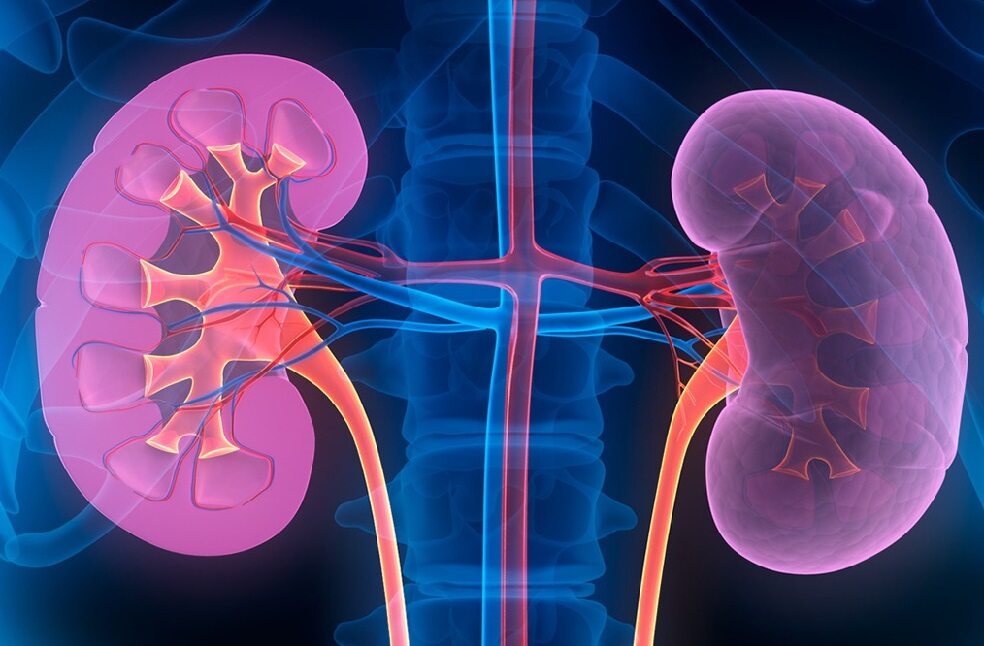
For a long time, scientists have been looking for alternatives, and many of them have been experimenting to see whether pig organs may be an option because they are anatomically similar to human organs. In the new study, scientists picked the Yucatan breed of pig because it has a similar weight to a human, and its kidney is also about the same size as a human’s.
“In the previous pig-to-primate donation experiments, scientists had to use a significant number of immunosuppressant drugs, which meant that the experiments would not be translatable to a human organ donation experiment,” researchers said. “But with this trial, the genetic modifications were effective enough that they needed only about as much medicine as a human could tolerate,” the research team added.
According to the authors, two additional gene edits seemed to be key to extending the monkeys’ lives in this study. The full combination of gene edits, combined with the immunosuppressive drugs, seemed to support what researchers considered long-term survival.

The team transplanted pig kidneys into more than 20 monkeys. None of the monkeys that got kidneys from the pigs without the seven human genes survived more than 50 days. The monkeys that got the full combination lived a lot longer. Five of them lived for more than a year, and one lived for more than two. The analysis showed that the single donated kidney seemed to perform as well as two natural kidneys.
“We’re the only group in the field to comprehensively address the safety and efficacy of our donor organ with these edits,” study co-author Dr. Mike Curtis, President and CEO of eGenesis, shared.
Mr. Curtis added that the study authors will work with the US Food and Drug Administration in the next few months to create a path to start clinical trials in humans.



